Introduction
When a blood artery in the brain bursts, bleeding inside or around the brain happens, resulting in a hemorrhagic stroke. Though it only makes up 15% of all stroke occurrences, this kind of stroke is more common in stroke-related mortality. The immediate and long-term treatment of hemorrhagic stroke is crucial in minimizing brain damage, improving survival rates, and enhancing recovery outcomes.
Definition
Treatment for hemorrhagic stroke, commonly referred to as cerebral hemorrhage, is marked by unusual bleeding that results from burst blood vessels in the brain. Generally speaking, managing hemorrhagic stroke entails blood pressure monitoring and drops. An additional surgical procedure to reduce blood pressure is part of the hemorrhagic stroke therapy. Healing from a hemorrhagic stroke is accelerated and more brain damage is prevented. By using a procedure called a “burr hole” to treat hemorrhagic strokes, there is a small chance of surgical intervention in the brain’s surrounding tissues.
Medical Interventions for Hemorrhagic Stroke
Stabilization and Supportive Care:
- Initial Stabilization: The first priority in treating a hemorrhagic stroke is stabilizing the patient. This includes maintaining airway, breathing, and circulation (the ABCs), monitoring vital signs, and ensuring the patient’s blood pressure is within a safe range.
- Supportive Care: Patients may require intubation and mechanical ventilation if they are unable to breathe adequately on their own. Oxygen therapy is often administered to maintain appropriate oxygen levels in the blood.
Blood Pressure Management:
- Hypertension Control: High blood pressure is a major risk factor for hemorrhagic stroke and can worsen bleeding. Careful management of blood pressure is essential to prevent further hemorrhage. Intravenous antihypertensive medications such as labetalol, nicardipine, or esmolol are often used to maintain blood pressure within a target range.
- Hypotension Avoidance: Conversely, it is also critical to avoid overly aggressive blood pressure reduction, which can reduce cerebral perfusion and worsen brain injury.
Reversal of Anticoagulation:
- Coagulopathy Correction: Patients who are on anticoagulant therapy, such as warfarin, heparin, or direct oral anticoagulants (DOACs), are at an increased risk of hemorrhagic stroke. Reversing anticoagulation right away is essential to stop bleeding that is still occurring.
- Reversal Agents: Specific reversal agents, such as vitamin K and fresh frozen plasma for warfarin, or andexanet alfa for factor Xa inhibitors, are administered to counteract the effects of anticoagulants.
Management of Intracranial Pressure (ICP):
- ICP Monitoring: Elevated intracranial pressure is a common complication of hemorrhagic stroke that can lead to brain herniation and death. ICP monitoring devices may be placed to keep track of pressure levels within the skull.
- Medications to Reduce ICP: Osmotic diuretics like mannitol and hypertonic saline are often used to reduce brain swelling and lower ICP. In some cases, sedatives and analgesics are administered to reduce metabolic demand and ICP.
Seizure Prophylaxis and Management:
- Antiepileptic Drugs (AEDs): Hemorrhagic stroke patients are at risk of seizures due to the irritation of brain tissue by blood. Prophylactic administration of antiepileptic drugs, such as phenytoin or levetiracetam, may be considered to prevent seizures.
Glucose Management:
- Blood Glucose Control: Hyperglycemia is common in stroke patients and can worsen outcomes by increasing the risk of infection and exacerbating brain injury. Careful management of blood glucose levels using insulin therapy is recommended to keep glucose levels within a normal range.
Management of Complications:
- Deep Vein Thrombosis (DVT) Prophylaxis: Patients who are immobilized due to hemorrhagic stroke are at risk for developing deep vein thrombosis. Mechanical prophylaxis, such as compression stockings or pneumatic compression devices, is used to prevent DVT, especially in the acute phase.
- Infection Prevention: Patients who have had a stroke are more vulnerable to infections, especially urinary tract infections and pneumonia. Preventive measures, including early mobilization, proper hygiene, and sometimes antibiotic prophylaxis, are important.
Surgical Interventions for Hemorrhagic Stroke
Craniotomy and Hematoma Evacuation:
- Indications for Surgery: Surgical evacuation of the hematoma may be necessary in patients with large, life-threatening intracerebral hemorrhages (ICH) or those with progressive neurological deterioration. Craniotomy involves opening the skull to remove the blood clot and relieve pressure on the brain.
- Timing of Surgery: The timing of surgical intervention is crucial and depends on the patient’s neurological status and the size and location of the hemorrhage. Early surgery may be beneficial in certain cases, but risks and benefits must be weighed carefully.
Minimally Invasive Surgery:
- Endoscopic Surgery: Endoscopic techniques allow for the removal of hematomas with smaller incisions and less disruption to surrounding brain tissue. This minimally invasive approach can be particularly useful for deep-seated hemorrhages that are difficult to access via traditional craniotomy.
- Stereotactic Aspiration: Stereotactic techniques involve using imaging guidance to precisely target and aspirate the hematoma through a small burr hole. This reduces the amount of harm to healthy brain tissue.
Decompressive Craniectomy:
- Indication and Procedure: Decompressive craniectomy involves removing a portion of the skull to allow the brain to swell without being compressed. This procedure is typically considered in cases of malignant cerebral edema following hemorrhagic stroke. After the swelling subsides, the skull is usually reconstructed in a second surgery.
- Outcomes: Decompressive craniectomy can be lifesaving, but it is associated with significant risks and may lead to long-term disability. Careful patient selection and timing are critical for optimizing outcomes.
Aneurysm Clipping or Coiling:
- Subarachnoid Hemorrhage Management: Hemorrhagic strokes caused by ruptured cerebral aneurysms, which result in subarachnoid hemorrhage (SAH), require specific surgical interventions. Aneurysm clipping involves placing a metal clip at the base of the aneurysm to stop the bleeding. Alternatively, endovascular coiling is a less invasive procedure in which coils are inserted into the aneurysm via a catheter to induce clotting and prevent further bleeding.
- Recovery and Prognosis: The choice between clipping and coiling depends on factors such as the aneurysm’s size, shape, and location, as well as the patient’s overall health. Both procedures have high success rates in preventing rebleeding, though long-term monitoring is required.
Arteriovenous Malformation (AVM) Resection:
- AVM Surgery: Arteriovenous malformations (AVMs) are abnormal tangles of blood vessels that can rupture and cause hemorrhagic stroke. Surgical resection of an AVM may be necessary to prevent future bleeding. This intricate process, which is often carried out in specialised facilities, calls for meticulous planning.
- Alternative Treatments: In some cases, stereotactic radiosurgery or endovascular embolization may be used as alternatives or adjuncts to traditional surgery for AVMs.
Post-Treatment and Rehabilitation
Neurological Rehabilitation:
- Rehabilitation Programs: Following acute treatment, patients with hemorrhagic stroke require comprehensive rehabilitation to regain lost functions. Physical therapy, occupational therapy, speech therapy, and cognitive rehabilitation are critical components of the recovery process.
- Goals and Outcomes: The primary goals of rehabilitation are to restore independence, improve quality of life, and prevent complications such as contractures and pressure sores. The extent of recovery varies depending on the severity of the stroke and the timeliness of interventions.
Long-Term Monitoring and Secondary Prevention:
- Regular Follow-up: Patients who have suffered a hemorrhagic stroke require ongoing monitoring to detect and manage potential complications, such as recurrent hemorrhage or hydrocephalus. Follow-up imaging examinations, such CT or MRI scans, are frequently utilised.
- Secondary Prevention: Preventive measures, including strict blood pressure control, lifestyle modifications, and adherence to prescribed medications, are essential to reduce the risk of future strokes.
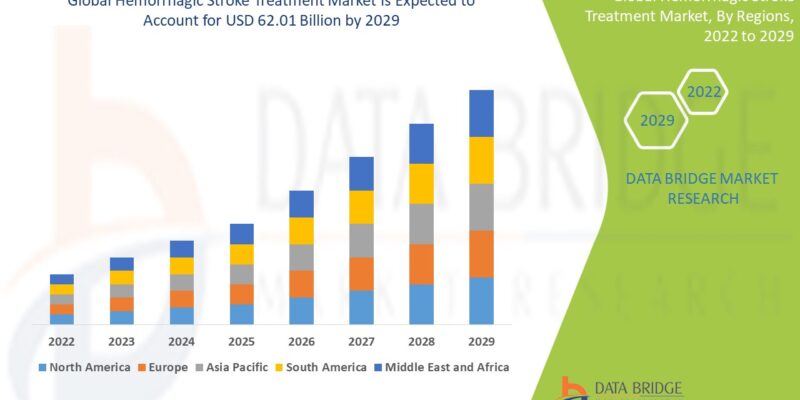
Growth Rate of Hemorrhagic Stroke Treatment Market
The global market for hemorrhagic stroke treatments is expected to increase at a CAGR of 2022–2029, according to Data Bridge Market Research. The market for hemorrhagic stroke treatments is anticipated to grow at a compound annual growth rate (CAGR) of roughly 7.80% over the projected period. It was estimated that the market would reach a valuation of USD 62.01 billion by 2029, from USD 34 billion in 2021.
Conclusion
Hemorrhagic stroke is a medical emergency that requires prompt and effective intervention to minimize brain damage and improve survival outcomes. A multidisciplinary approach, combining medical and surgical treatments, is often necessary to manage the complex challenges associated with this condition. Early recognition, rapid stabilization, and appropriate intervention are key to achieving the best possible outcomes for patients affected by hemorrhagic stroke.